Tuesday, October 28, 2008
Glaucoma & Thyroid disease
Hypothyroidism "may lead to the deposition of mucopolysaccharides in the trabecular meshwork, which increases IOP as well as aqueous outflow resistance"
Tuesday, October 14, 2008
Work up for Optic Neuropathy
- CBC
- C-reactive protein (GCA)
- ESR (GCA)
- Platelet count
- Lyme titer (infectious)
- ANA with reflex titer (rheumatologic)
- ACE (sarcoid)
- RPR (syphillis/infectious)
- FTA-ABS (syphillis/infectious)
- Vitamin B12 (nutritional)
- Folic acid (nutritional)
- Methylmalonic acid (occult vitamin B12 deficiency)
- MRI (preferred) or CT scan
- a young patient complaining of sudden vision loss will more likely have an optic neuritis (ON)
- a middle-aged person would more likely have nonarteritic anterior ischemic optic neuropathy (NAION).
- an older patient with the same complaint would more likely have arteritic anterior ischemic optic neuropathy (AAION) associated with giant cell arteritis (GCA).
- NAION: no pain, “disk-at-risk” appearance in the fellow eye (small, crowded optic disc with little or no cupping that is predisposed to the ischemic process of NAION), less pale nerve
- AAION: pain with eye movements, optic nerve dema usually associated with hemorrhages during the acute phase, more pale nerve
- AAION and GCA symptoms: jaw claudication, scalp tenderness, fatigue, loss of appetite and fever.
- ON: pain on eye movement; you will see either a normal optic disc (retrobulbar optic neuritis) or disc swelling without hemorrhages (papillitis).
- Multiple sclerosis (MS) symptoms: weakness, numbness, pares-thesias or any other neurologic symptoms.
- Traumatic optic neuropathy: pallor of the neuroretinal rim suggests a longstanding or chronic process
- Structural abnormality or mass: non-acute, nonglaucomatous optic neuropathy; patient is in need of neuro-imaging to look for either a structural abnormality such as a mass or abnormal enhancement indicating an inflammatory process, or some form of disruption of the blood-brain barrier.
- GCA: A CBC, ESR, C-reactive protein and platelet count must be performed on patients over the age of 50
Sinusitis
Clinical Features
- stuffy nose, followed by the slow onset of increased sinus pressure
- malaise, toxicity, headache, possibly a slightly elevated temperature, and usually a normal WBC count.
- as the disease progresses over two to three days, symptoms become more pronounced and severe.
- associated pain to the eye and orbit is a constant, dull ache with no throbbing. It may worsen if the patient bends over, coughs or strains.
- patients with chronic sinusitis usually have: allergic rhinitis, which is signaled by itchy/watery eyes, seasonal variation in symptoms and a family history of the disorder.
- acute sinusitis symptoms: facial pain or tenderness, colored nasal discharge, headache, decreased sense of smell, maxillary toothache, cough (usually daytime), fever, malodorous breath and occasional periorbital swelling. Less common findings include middle ear effusion, swelling of the face and nasal bleeding.24
- ethmoid sinusitis: headache is a prominent symptom, located either behind or between the eyes with radiation to the temporal region. The eyes may be tender to pressure, and extreme tenderness on palpation of the medial and superior aspects of the orbit may be present. The patient may experience discomfort with eye movement.
- frontal sinusitis: may cause a frontal headache, which radiates behind the eyes to the vertex of the skull. The pain is generally constant and tends to feel like a pressure sensation. There is also point tenderness on the undersurface of the medial aspect of the superior orbital rim, which is the floor of the frontal sinus. Often, the pain is not present in the early morning after a night of rest. It usually appears one or two hours after waking, increases for three or four hours and becomes less severe in the late afternoon or evening. Apply finger pressure upward toward the floor of the sinus, where the sinus wall is thin, or perform palpation directly over the frontal sinus. Swelling caused by tumors or retained secretions (mucoceles) may cause a downward bulge in the floor of the frontal sinus. Transillumination of the frontal sinuses is done by placing a light source below the supraorbital rim, under the floor of the frontal sinus, at the upper inner angle of the orbit. This technique helps assess light transmission into the lower forehead.
- sphenoid sinusitis: causes pain at the occiput or vertex, yet frontotemporal, retro-orbital or facial pain is more common. It may also travel from the orbit to the mastoid area. The pain is described as constant, and if it occurs retrobulbarly, quite severe. This type of severe retro-orbital pain can cause photophobia and tearing.
- maxillary sinusitis: 10% of maxillary sinusitis is generally secondary to dental root infection. Simultaneous finger pressure over both maxillae exemplifies differences in tenderness.Perform transillumination by placing the light source over the middle of the infraorbital rim.
Examination and Testing- thorough patient history and physical examination to establish either acute or chronic sinusitis
- an evaluation of vision, pupils, extraocular muscle function, exophthalmometry, slit lamp and funduscopy helps identify any secondary periorbital, orbital or ocular complications
- evaluation of the head and neck should be performed.
Amaurosis Fugax
-Patients usually have a history of hypertension, diabetes or hypercholesterolemia; danger of cerebral vascular accident (CVA) in addition to ocular sequelae.
-patients must be referred to the emergency room to rule out emboli actively being thrown from the carotid artery, cardiac valves or aortic arch.
-If a patient with these symptoms is 56 or older, one must consider giant cell arteritis (GCA)
-Other conditions, such as antiphospholipid antibody syndrome and systemic lupus erythematous, may also result in arteriole occlusion
-A central artery occlusion of less than 24 hours might be aided by intervention, including lowering IOP, performing ocular massage and attempting vasodilation by increasing carbon dioxide levels in the blood (this is accomplished by having the patient breathe into a paper bag).
-r/o weakness, numbness, headache or speech difficulty
-lab w/u:
- emergent complete blood count (CBC) with differential
- prothrombin time (PT)
- partial thromboplastin time (PTT) tests
- platelets
- carotid duplex
- echocardiogram
-educate to report immediately to the ER if any non-recovering vision loss or peripheral weakness or numbness
Saturday, July 19, 2008
Oral medical therapies
Oral Antibiotics
- Penicillins
- Augmentin (amoxocillin + clavulanic acid)
- 500mg, 875mg, or 1,000mg b.i.d. x 1 week (depending on severity)
- The dosage is determined by the severity of the clinical condition.
- Cephalosporins --5% to 10% cross-sensitivity with PCN
- Keflex (Cephalexin)
- 500mg b.i.d. x 1 week
- Macrolides -- only for pregnancy or chlamydia
- erythromycin
- 500mg t.i.d. x 1 week
- safe for pregnancy
- azithromycin
- 250mg tablets, 500mg tablets, 1,000mg oral suspension
- Zmax, a 2,000mg extended-release oral suspension
- chlamydial infection: one dose of either 1,000mg or 2,000mg azithromycin
- Fluoroquinolones (usually reserved for PCN allergies)
- Levaquin (Levofloxacin)
- 500mg q.d. x 1 week
Oral Corticosteroids
- best taken with meals to minimize the risk of GI upset
- caution: diabetes or peptic ulcer disease
- oral steroids exacerbating peptic ulcers
- a proton (hydrogen) pump inhibitor (PPI) can be prescribed, which will either fully protect or greatly diminish any expression of gastric ulceration
- PIs simply and safely reduce gastric acid secretion
- Prilosec (OTC, 20mg capsules, swallowed whole before a meal once daily), Nexium, Prevacid for the duration of the steroid therapy and for one additional week.
- patients with diabetes are prone to lose glycemic control while on oral steroids
- type II may well have increased blood glucose levels for a few days, which is rarely a problem; glycemic control returns after cessation of the steroid
- type I diabetes, they should be instructed to adjust their insulin dosagethe duration of their therapy
- 1,000mg of methylprednisolone (500mg q12 hours) IV daily for three days
Episcleritis
- Lotemax or FML q.i.d. x 1 week, then b.i.d. x 1 week, and that’s it
- For stubborn cases, add 40mg of p.o. prednisone x 2 days, then 30mg x 2 days, then 20mg x 2 days (up to six days), then 10mg x 2 to 4 more days
- rarely are systematic laboratory studies indicated
- if there are multiple recurrences or if the presentation is difficult to suppress. Lab work-up:
- Rheumatoid arthritis: Rheumatoid factor (RF) and antinuclear antibody (ANA)
- Systemic lupus erythematosus: Antinuclear antibody (ANA) and anti-DNA antibody
- Gout: Serum uric acid
- Syphilis: FTA-ABS, VDRL, MHA-TP or RPR
- Wegener’s granulomatosis: Antineutrophil cytoplasmic antibody (ANCA).
- Acne rosacea: None. This is a clinical diagnosis.
- idiopathic white blood cell infiltration resulting in chemosis (without itching, therefore not allergic), proptosis, eyelid edema, and occasionally diplopia (because of orbital congestion)
- send patients for a CT scan to rule out any other orbital process, and to confirm our clinical diagnosis
- unusual or atypical eyelid or orbital presentation, order a CT scan
- if strongly feel the condition is infectious, start Augmentin 875mg b.i.d. or, if penicillin-allergic, Levaquin 500mg q.d.,
- Orbital pseudotumor is treated with 60mg p.o. prednisone x 3 to 4 days, then 40mg x 3 to 4 days, then 20mg x 1 to 2 weeks, then 10mg x 1 to 2 weeks
Marked or stubborn iridocyclitis
- If, after a few days of aggressive use of Pred Forte and a therapeutic cycloplegic (with perhaps FML ointment h.s.), the iritis appears unyielding (and the patient is compliant with the medications), try augmenting the topical medications with oral prednisone
- consider starting at 40mg a day x 2 or 3 days, 30mg x 2 or 3 days, and then reevaluate the patient. Assuming good improvement, continue the topical assault and continue to reduce the p.o. prednisone to 20mg x 1 week and recheck the patient. Assuming continued progress, stay the course topically, and reduce the p.o. prednisone to 10mg q.d.x 1 week and recheck the patient. This iritis should be very well controlled.
- Now the topical taper can begin. Reduce the Pred Forte to q2 hours x 1 week, and stop the FML ointment now, or after one more week. If the condition continues to improve, then continue q.i.d. x 1 week and recheck the patient. At this point, there should be little or no anterior chamber evidence of iritis. Keep this patient at b.i.d. for another 1 to 2 weeks.
- Regarding the cycloplegic agent, stop it when the cells and flare are reduced to Grade I or less
- If the IOP becomes elevated 10mm Hg or more from baseline, consider adding beta-blocker once daily if there are no contraindications, or brimonidine 0.2% q12 hours
- Once the inflammation is controlled and the patient is a steroid responder, switch the medication to Lotemax to finish the corticosteroid component of the therapy.
- If the iritis rebounds when the oral steroid is reduced below 20mg q.d., add a COX-2 inhibitor such as Celebrex (celecoxib, Pfizer) 100mg or 200mg b.i.d., or ibuprofen 400mg q.i.d. can be beneficial. In this scenario
- add one of these non-steroidals to the 20mg of oral prednisone q.d. x 1 week and then begin tapering the oral prednisone to 10mg q.d. x 1 week (or two) while concurrently using the oral NSAID.
- Many times, the use of NSAIDs in such instances enables the completion of the oral prednisone taper as planned. Once off the oral prednisone, continue the patient on the NSAID for a couple more weeks.
Bell's Palsy
- prednisolone 60mg a day for a few days, then tapering to 40mg, 20mg, and 10mg, depending upon the clinical response
- acyclovir 400mg five times a day for one week, or valacyclovir (Valtrex, GlaxoSmithKline) 500mg three times a day for one week, or famciclovir (Famvir, Novartis) 250mg three times daily for one week
- there is indecision regarding the need for such oral antiviral therapy in the setting of Bell’s palsy, however
- the current thinking is to prescribe an antiviral if the condition is severe or complete.
- preserve and maintain ocular surface integrity with frequent lubrication with a preservativefree artificial tear such as TheraTears Liquid Gel, or a gel formulation such as GenTeal Gel
- If more aggressive lubrication is required, an ointment such as Refresh P.M. can be employed
- modypatients fully recover in three to nine months.
- no effective topical therapy to enhance meibomian gland function beyond warm soaks, lid scrubs and glandular massage.
- Doxycycline can exert a beneficial effect on the secretory function of these glands
- two 50mg capsules daily for two weeks (as a loading dose), then just one 50mg capsule daily x 3 to 6 months or longer, depending upon the clinical response. (read “Meibomian Gland Dysfunction,” by P.J. Driver, et al., in Survey of Ophthalmology, March-April 1996)
- side effects: occasional vaginal candidiasis
- OCuSOFT: ALODOX™ Convenience Kit
Allergic Blepharodermatitis
- usually just cold compresses and/or 0.1% triamcinolone cream applied b.i.d. to q.i.d.
- add oral prednisone p.r.n., or, depending upon your clinical judgment, prescribe oral prednisone as initial therapy, with or without concurrent topical steroid cream.
- the more severe the blepharodermatitis (or greater surface area involvement), the more we lean toward oral therapy.
- Fortunately, these conditions tend to resolve with only two to four days of therapy. We generally prescribe 40mg q.d. x 2 days, then 20mg q.d. x 2 to 4 more days, and then stop. There is no reason to taper such a low dose or short course of oral prednisone any further
- Tetracyclines and corticosteroids can improve tissue adhesion of the basal epithelium/Bowman’s membrane/anterior stromal complex
- 50mg tablets of doxycycline to be taken by mouth as one 50mg tablet p.o. b.i.d. x 2 weeks, then q.d. x 6 to 8 weeks
- concurrently prescribe Lotemax q.i.d. x 1 month, then b.i.d. x 1 month
Oral Antivirals
- Acyclovir is available in 200mg capsules, 400mg and 800mg tablets, and in a 200mg-per-teaspoon (5ml) banana-flavored oral suspension
- Valtrex comes in 500mg and 1,000mg tablets
- Famvir is available in 125mg, 250mg and 500mg tablets.
- Acyclovir and Valtrex arePregnancy Category C; Famvir is Category B.
- precautions: kidney function, as all of the antiviral drugs are eliminated via the urine; ask patients about any known renal disease.
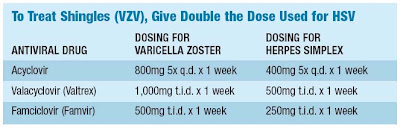
Herpes Zoster
- herpes zoster ophthalmicus 50% of the time
- keratitis, inflammatory anterior uveitis (or both), and less commonly as episcleritis and trabeculitis (which can result in high IOP).
- treated aggressively with topical corticosteroids such as Lotemax or Pred Forte.
- Oral antivirals can be used to treat childhood chickenpox, if indicated. The FDA/CDC recommended dosage for treating chicken pox in children over age 2 weighing at least 40 pounds can be as much as acyclovir 800mg q.i.d. x 5 days (the dosage for shingles is 800mg 5 times a day for 7 days).
- patient presenting with ophthalmic division shingles: standard dosage is acyclovir 800mg p.o. 5 times a day x 7 days, and potentially up to 10 to 14 days p.r.n. The clinically equivalent dosage for Valtrex is 1,000mg p.o. t.i.d. x 7 days. For Famvir, the dosage is 500mg p.o. t.i.d. x 7 days.
Herpes Simplex
- primary herpetic dermatitis to the face and/or eyelids. The cornea is not usually involved, but can be. In either case,
- 400mg of acyclovir 5 times per day x 7 days, Valtrex 500mg t.i.d. x 7 days, or Famvir 250mg t.i.d. x 7 days.
- HSV keratitis: supplement the oral antiviral with preservative-free artificial tears.
- Concurrent topical trifluridine is rarely ever needed
- Certainly, if in a few days the ocular dermatitis is resolved and the keratitis is unchanged, then adding topical Viroptic q2 hours x 4 days, then q.i.d. x 4 days may be needed, but this would be highly unusual.
- eye-related pain, which can certainly be intense, is invariably short-lived
- ask patients what they generally use for pain (extra-strength acetaminophen and ibuprofen)
- Acetaminophen (Extra Strength Tylenol) is indeed an excellent analgesic, which also has antipyretic (fever-reducing) properties
- is synergistic with oral narcotic analgesics
- Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen are likewise very broadly used and are generically available.
- Ibuprofen is available over-the-counter as 200mg tablets or capsules.
- The optimum dosage of ibuprofen is 1,600mg per day. It is most often dosed as two 200mg tablets taken every four hours. This dosage is generally sufficient and approximates that of a Schedule III opioid.
- Tylenol #3 (30mg of codeine and 300mg of acetaminophen.)
Fish oil
- support body's natural inflammatory response
- support tear production
- protect eyes from oxidative damage
1g = advanced support for healthy eyes
2-3g = for high intesnity eye support/dry/red/itching/painful eye
Tuesday, June 24, 2008
Corneal dystrophies

- autosomal dominant
- presents in 1st decade and progresses into adulthood
- diffusely distributed intraepithelial cysts that are usually concentrated in the interpalpebral zone
- in severe cases cysts can rupture on surface causing irritation and photophobia (use bandage CL)
- autosomal dominant or due to trauma or surgery
- geographic epithelial changes (maps), opaque irregularities (dots) or concentric irregular lines (fingerprints)
- results from a thickened basement membrane
- can result in recurrent corneal erosions (bandage CL)
- Muro 128 during the day or ung at night may be necessary for up to 3 months (if this fails to prevent recurrent erosions, may need anterior stromal puncture or PTK
- autosomal dominant, presents 1st decade of life
- subepithelial reticular changes that progress until middle age
- may opacify or induce irregular astigmatism
- may have erosions (bandage CL)
- autosomal dominant, presents 1-2nd decade of life
- grayish white opacities form in the central (almost never periphery) anterior stroma with clear intervening space
- lesions can become larger and more numerous with stromal hazing
- rarest (autosomal recessive)
- anterior stroma becomes hazy in 1st decade, progressing to opacified lesions
- more likely to affect peripheral cornea
- worse visual prognosis
- autosomal dominant, 1st decade
- refractile lines in the anterior stroma which eventually branch and develop deeper into stroma (lattice design)
- prone to erosions (bandage CL)
- vesicles deep into the cornea that may be isolated, mutiple/coalesced, or broad bands/train tracks
- may apear blister-like and have a gray white halo aroudn them
- increased risk of glaucoma
- guttata (refractice excrescenses) on posterior cornea due to abnormal functioning endothelial cells (from aging, trauma or inflammation)
- Fuch's is diagnosed when nonfunctioning endo causes corneal edema
- vision worse upon awakening
- muro 128 gtts and ung
- extreme epithelial edema may cause bulae with pain and photophobia (bandage CL)
- usually have cataracts
- cataract surgery may cause a dramatic worsening of Fuch's
BANDAGE CL
- use steeper curve (unless there is no mvmt then use flatter one)
Monday, June 23, 2008
Cross-cylinder calculators
- http://www.aoa.org/x4783.xml
- procare.cibavision.com
- coopervision.com
- ecp.acuvue.com
- eyedock.com
Thursday, May 22, 2008
Online learning center
http://learning.coopervision.com/
Acuvue2 colors: https://www.jnjvision.com/imakeover/
Freshlook contacts: http://www.freshlookcontacts.com/
Resolving dry eye in RGP wearers
- when the corneal surface isn't adequately resurfaced with tears after the blink
- edge of GP lens holds lid away from corneal surface during blink
- incomplete blinking
- may see vascularized limbal keratitis
Adjusting the fit to minimize excessive edge lift and inferior position
Strive for superior lens position by:
- decreasing diameter
- reduce CT
- +/- lenticulars
- reduce edge clearance
- steepen PC radius
- narrow PC width
- reduce edge thickness
Patient CL compliance handout from AOA
http://www.aoa.org/x8024.xml
Thursday, April 10, 2008
Vogt-Koyanagi-Haraa (VKH) syndrome
- bilateral granulomatous panuveitis associated with serous retinal detachments, optic disc edema, neurologic abnormalities and skin pigment changes
- systemic manifestations: tinnitus, vitiligo, alopecia, headache and meningismus
- T cell-mediated autoimmune process directed against melanocyte antigens
- more prevalent in Asians, Latinos and American Indians
- women slightly > men
- any age but usually 4th-6h decades of life
- prodromal
- acute uveitic (poor VA, severe AC inflammation w/ or w/o posterior synchiae)
- convalescent
- chronic recurrent (RPE alterations, widespread loss of choroidal melanocytes producing a sunset-glow fundus and choroidal Dalen-Fuchs-like nodules, cutaneous vitiligo, poliosis and alopecia)
- catarct, glaucoma, CNV, subretinal fibrosis, ERM, macular atrophy
- prompt initiation of high-dose systemic corticosteroid therapy (1 to 1.5 mg/kg/day) concurrent with a corticosteroid-sparing immunosuppresive agent) , tapering patients off within 2-3 months
- rapid and aggressive treatment is important to minimize disease duration and lessen the risk of progression into a chronic recurrent form of disease and reduce the incidence of systemic and ocular complications
Lagophthalmos evaluation/treatment
Taking the history
recent trauma or surgery involving the head/face/eye
past infections e.g. herpes zoster
past symptoms suggestive of thyroid disease or obstructive sleep apnea
Testing the lids and globe
ask patient to look down and gently close both eyes
lagophthalmos is present when a space remains b/w the upper and lower eyelid margins in extreme downgaze
measure this space with a ruler
record the blink rate an the completeness of blink
test cranial nerve function (pay attention to ocular motility and the strength of the orbicularis oculi muscle by evaluating the force generated on attempted eyelid closure)
presence and quality of Bell's phenomenon should be noted (cornea is better protected when the eye rolls upward on attempted closure of the eyelids)
Testing the cornea
test corneal sensitivity by applying soft cotton to the unanesthetized cornea and comparing the blink reaction with that of the fellow eye
describe presence of PEE with NaFl
record TBUT
Etiology
Facial nerve (VII)
- innervates frontalis muscle (raises the eyebrow) and the orbicularis oculi muscle (closes the eyelid)
- loss of function of the VII nihibits eyelid closure, blink reflex, and lacrimal pumping mechanism
- also innervates the muscles of facial expression including the zygomaticus (elevate the cheeks) and corrugator supercilii and procerus (depress the eyebrow) which help facial symmetry
Trauma
- VII is susceptible to blunt trauma or laceration along it's bony course
- fractures to the skull base or mandible can damage the nerve or one of its branches
- neurosurgical procedures
Cerebrovascular accidents
- VII receives its blood supply from the anterior inferior cerebellar artery (susceptible to ischemic damage)
Bell's Palsy
- idiopathic VII palsy thought to be associated with an acute viral infection or reactivation of herpes simplex virus
Tumors
- acoustic neuromas in the cerebellopontine angle and metastatic lesions are most commonly associated with lagophthalmos
- need MRI with gadolinium
Infections, immune-mediated causes
- less common causes: Lyme disease, chickenpox, mumps, polio, Guillain-Barre syndrome, leprosy, diphtheria and botulism
Mobius' syndrome
- rare, congenital condition with CN palsies (esp. VI and VII), motility disturbances, limb anomalies and orofacial defects
Eyelids
damage or degeneration of any of the eyelid tissue structures (skin/subcutaneous tissue, orbicularis oculi muscle, orbital septum, orbital fat, muscles of retraction, tarsus, conjunctiva) may inhibit good eyelid closure
Cicatrices- chemical or thermal burns
- ocular cicatricial pemphigoid
- Stevens-Johnson syndrome
- mechanical trauma
- above may cause scarring of the soft tissues or retractor muscles
- excessive removal of eyelid skin or muscle (blepharoplsty, tumor excision)
- overcorrection in ptosis repair
- exophthalmos in thyroid ophthalmopathy
- aquired causes (orbital blowout fractures, orbital fat atrophy from trauma, infection, inflammation, aging or wasting disease such as linear scleroderma or HIV-AIDS)
- phthisical or prephthisical eye
- scirrhous carcinomas leading to contraction of orbital fat
- result of severe laxity and flexibility of the superior and inferior tarsal plates
- may be associated with obstructive sleep apnea
Symptoms
- FBS and tearing
- pain in AM from increased corneal exposure and dryness during sleep
- blurry vision from unstable TF
Work-up and treatment
- Medical treatment and supportive care for the cornea (non-preserved artifical tears at least QID, ointments QHS/PRN, moisture gogles, methylcellulose)
- Tarsorrhaphy (suturing lateral 1/3 of eyelids, temporary or permanent)
- Gold weight implantation (gold is inert and doesn't show through thin skin of eyelid)
- Uper eyelid retraction and levator recession (for lagophthalmos due to thyroid ophthalmopathy)
- Lower eyelid tightening and elevation (tightenting procedure will improve apposition fo the lower eyelid to teh globe and decrease tearing)
- Ancillary surgical procedures (facial surgery)
Tuesday, March 25, 2008
Myasthenia Gravis
- autoimmune disorder in which antibodies prevent the neurotransmitter acetylcholine from attaching to muscle receptors, thereby interfering with muscle contractions
- characterized by fatigability of voluntary eye movements (diplopia worsens as day progresses, improves with sleep)
- can present with diplopia, ptosis or both
Tests
- sustained upgaze: patients will show a gradual worsening as the levator muscle fatigues
- ice pack test: apply a cold pack to the eyelid for 5 minutes (cold temp allows Ach to have more time to react with the muscle receptors), check for improvement in ptosis
- sleep test: have the patietn take a nap in the exam chair for 30-45 minutes, check for improvement in ptosis
- Tensilon is an IV cholinergic drug that typically shows improvement in muscle function within seconds
Treatment
- Mestinon (cholinergic drug) and immunosuppresive therapy (neurophthalmology)
- if medications don't eliminate ptosis/diplopia, may try prismatic corrections and ptosis crutches
Differentials
- 3rd nerve palsy: has vertical and horizontal component
- skew deviation: usually appears with concomitant hypertropia and other abnormal eye movements such as nystagmus
- disease of the orbit: neoplastic, inflammatory, infectious, traumatic can cause proptosis, lid retraction, periorbital edema, conjunctival hyperemia, disc edema
Thursday, March 6, 2008
Determining Prism
- Prism needed = 2/3 (phoria) - 1/3 (compinsating fusional vergence)
- eg: pt has 6 XP and BO to blur is 6, the prism needed is 2/3 (6) - 1/3 (6) = 2 BI
Percival's criterion
- Prism needed = 1/3 (greater limit of BI or BO range) - 2/3 (lesser limit of BI or BO range)
- eg: pt has 6 XP and BO ranges of 6/10/8 and BI range of 21/26/22, prism needed = 1/3 (21) - 2/3 (6) = 3 BI
Parks-Bielschowsky Three Step Test (for head tilts "torticollis")
- Which eye is hyper in primay gaze?
- In which horizontal gaze does hyperdeviation increase?
- In which direction of head tilt does the hyperdeviation increase?
- right hyper --> right gaze --> right tilt = LIO
- right hyper --> right gaze --> left tilt = RIR
- right hyper --> left gaze --> right tilt = RSO (most common cause of vertical dipl.)
- right hyper --> left gaze --> left tilt = LSR
- right hyper --> right gaze --> right tilt = RSR
- right hyper --> right gaze --> left tilt = LSO (most common cause of vertical dipl.)
- right hyper --> left gaze --> right tilt = RIR
- right hyper --> left gaze --> left tilt = RIO
Postures and Treatments
- Left head turn --> Right gaze preferred --> LLR or RMR paresis --> give yoked prism base left
- Right head turn --> Left gaze preferred --> RLR or LMR paresis --> give yoked prism base right
- Left head tilt --> Right hyperdeviation --> RSO paresis (most common cause of vertical diplopia)--> BD over right eye if longstanding
- Right head tilt --> Left hyperdeviation --> LSO paresis (most common cause of vertical diplopia)--> BU over left eye if longstanding
- Head tip back --> Downgaze preferred --> V-pattern exotropia or A-pattern esotropia --> BU yoked prism
- Chin depressed --> Upgaze preferred --> A-pattern exotropia or V-pattern esotropia --> BD yoked prism
Coding Dry Eye
Ocular findings:
- Tear film insufficiency (375.15) -- test show decreased TF; for punctal plugs diagnosis
- Keratoconjunctivitis sicca, not specified as Sjogren's (370.33) -- observation of "inflammation of the conjunctiva and cornea, characterized by "horny"-looking tissue and excess blood in these areas"
- Punctate keratitis (370.21)
- Exposure keratitis (370.34)
- Sjogren's syndrome (710.2)
Patient symptoms:
- Eye pain (379.91) -- may be used for all levels of eye discomfort, e.g. burning/stinging
- Redness of eyes (379.93) -- r/o episcleritis (379.01) and scleritis (379.00)
- Epiphora (375.20) -- dry eye due to reflex tearing
Procedure diagnastic codes:
- External ocular photography (92285) -- photos need to document the efficacy of treatment or the progression of the disease, and not just enhance the medical record or billable procedures
- Bandage contact lenses (92070) -- covers fitting and supply of lens
Monday, February 25, 2008
Flaxseed oil/Dry eye supplements
- MGD/blepharitis
warm compresses/lid scrubs bid
Zylet qid x 1 week, bid x 1 week
- oral antibiotics
- nutritional supplements
- dry mouth therapies
Hydrate (OcuSoft)
BioTears fish oil supplements
Lovaza (omega-3)
1,000-1,500mg per day of each
4-6 weeks before response (including better skin and hair)
TheraTears nutrition supplements for patients with intestinal sensitivities
Alodox convenience kit (doxy 20mg + ocusoft lid scrubs), take with water, don't take with calcium (negates drug)
Sjogren's syndrome
- most age >40
- women 9x > men
- dry eye, dry mouth, autoimmune disorder
- lid hygiene/massage for MGD, AT, Restasis, steroids
- oral Minocycline 50mg bid x 2 weeks then 50mg qd x 1 month, then taper (usually 8 weeks to work); side effects: stained teeth, vaginitis, photosensitivity
- or Doxycycline 50mg bid x 1-2 months then qd x 1 month (side effects: photosensivitiy, sensitivity to dair products/antacids)
- or Periostat (20mg doxy) bid x 1-2 months then qd x 1 month
- Salagen and Evoxac (30mg tid) drugs that stimulate the salivary glands to produce saliva
1. Ocular symptoms:
- daily, persistent, troublesome dry eyes >3 months
- recurrent sensation of sand or gravel in the eyes
- use AT more than tid
- daily feeling of dry mouth for >3 months
- recurrent or persistently swollen salivery glands
- need to drink liquids to aid in swallowing dry food
- Schirmer's test w/o anesthesia (<5>
- Rose bengal or other dry eye findings
- focal lymphocytic sialoadentitis in minor salivary glands, evaluated by histopathologist
- unstimulated whole salivary flow (<1.5>
- parotid sialography showing diffuse sialectasias without evidence of major duct obstruction
- salivary scintigraphy showing delayed uptake, reduced concentration and/or delayed excretion of tracer
- presence of antibodies to Ro(SSA) or La(SSB) antigens or both
- any 4 of the 6 items as long as item 4 or 6 is positive
- presence of any 3 of 4 objective criteria items (3 thru 6)
- in patients with a potentially associated disease (e.g. connective tissue disease, RA, lupus) with the presence of item 1 or 2 plus any two from items 3-5
Posner-Schlossman sydrome (glaucomatocyclitic crisis)
- repeated attacks of a mild cyclitis with significantly elevated IOP, usually unilateral
- asymptomatic or may have symptoms of sudden onset of blurred vision, mild pain and haloes around lights
- signs: mild anterior uveitis and high IOP (40-60), may have KPs w/ corneal edema, gonio open angle, mild degree of iris heterochromia and anisocoria (involved pupil larger)
- usually occurs b/w age of 20-50
- unknown etiology (possible allergy, viral infection such as CMV or herpes simplex, stress-induced)
- inflammatory material or precipitates on the TM reduce aqueous outflow or trabeculitis causes decreased outflow
- acute and self-limiting (resolves or without treatment), lasting hours to weeks
- associated with POAG and NAION in patients with small, crowded optic nerves
- treatment: control inflammation -- topical corticosteroid may be used alone or with IOP med (e.g. PF 1% qid qid with alphagan tid); don't use miotics or prostaglandins; no need for medication b/w episodes
- medical work-up: Chest x-ray, bilateral plain radiographs of ankles, feet and sacroiliac joints (to check for joint abnormalities), CBC with differential, ESR, TSH, HLA-B27, CRP, RF, ANA, Chorionic gonadotropin, RPR, Lupus
Reis-Buckler's dystrophy
- bilateral
- causes photophobia, corneal erosions and subepithelial and anterior stromal scarring
- multiple subepithelial ring-shaped opacities (honeycomb apperance) in the centre of the cornea corneal surface is irregular with ferritin deposition
EBMD
Band keratopathy
Due to:
- hypercalcemia 2^ hyperparathyroidism, excessive vitamin D intake,
renal failure, hypophosphatasia, milk-alkali syndrome, Paget disease,
sarcoidosis - topical medications that contain phosphates (steroid phosphates,
pilocarpine) - chronic ocular inflammation (uveitis, end stage glaucoma) causes elevation
of the surface pH out of the physiologic range which changes the solubility
product and favors precipitation - compromised endothelial function and corneal edema (2^ silicone oil from RD surgery)
- serum calcium and phosphate level
- if sarcoid is suspected, an angiotensin-converting enzyme (ACE) should be obtained
- parathyroid hormone levels
Salzman's Nodular Degeneration
- peripheral elevated subephithelial nodules and irregular astigmatism
- needs smaller diameter GPs to try to keep the leses away from the peripheral nodules
Terrien's Marginal Degeneration
- progressive thinning of the peripheral corneal (usually S/T)
- increases regular and irregular against-the-rule astigmatism
- needs larger GP lens diameters to prevent decentration
Nutrition in AMD
- verteporfin(Visudyne)
- pegaptanib (Macugen)
- Lucentis
- Avastin
- 10% rate of conversion from dry to wet AMD
- nutritional supplementation decreases risk
- oxidation hypothesis: breakdown of antioxidant systems and generation of free radicals damages lipid membranes; antioxidant deficiency may predispose patient to disease
AMD and cardiovascular disease
- shared risk factors: elevated lipids, cholesterol, CRP, arteriosclerosis, cigarette smoking, inflammatin, HTN
- category 1 or 2 (little-to-no AMD or few small drusen): risk of developing wet AMD at 5 years = 1.5%
- category 3 (large intermediate-size drusen or nonvoeal geographic atrophy): risk of developing wet AMD at 5 years = 20%
- category 4 (at least 1 eye with wet AMD or foveal geographic atrophy)
- if wet AMD present in one eye, risk to the fellow eye is 45%
- risk for vision loss at 5 years: antioxidant + zinc = 20% reduction in risk
- risk for progression to wet AMD at 5 years: antioxidant + zinc or zinc alone = 25% reduction in risk
- recommendations: patients with intermediate to advanced AMD (category 3 or 4) should take daily supplemental theraphy
- people who smoke should avoid beta carotene due to increased risk of lung cancer
- study of lutein, zeaxanthin, omega-3 fatty acids
- lutein and zeaxanthin are natural carotenoids found in macula; antioxidants; filters of UV light; play role in structural signal transduction; macular pigment decreases with age; decrease predisposes patient to increased rsik for AMD
- zeaxanthin can increase macular pigment
- 6m lutein associated with reduced risk for develping AMD by up to 43%
- higher body mass index associated with greater AMD risk
- high intake of fat in prcessed baked gods increases odds for developing wet AMD by 2.4
- other sources of fat (nuts) protective
- lutein, zeaxanthin, and omega-3 fatty acids not produced by body
- high intake of omega-3 fatty acids protects against wet AMD (dose-dependent)
- omega-3 fatty acids in broiled or baked fish: dose-dependent decrease in risk for AMD progression
Side-effects/interactions
- high levels of beta-carotene linked to increased incidence of lung cancer among heavy smokers
- high volumes of zinc linked with genitourinary and GI disorders
Tuesday, February 19, 2008
Dosing guides
http://pconsupersite.com/pdfs/0709guide.pdf
Topical allergy medications:
http://pconsupersite.com/pdfs/0802guide.pdf
Topical glaucoma medications:
http://pconsupersite.com/pdfs/0705guide.pdf
Tuesday, February 12, 2008
Pellucid marginal degeneration
- bilateral asymmetric focal ectasia of the corneal stroma 1-2mm above the inferior limbus b/w 5 & 7 o'clock w/o evidence of scarring, vascularization or lipid infiltration
- progressive ectasia results in the development of ATR astigmatism
- can lead to corneal hydrops
- advanced cases show "kissing doves" or "crab claw" topography with superior flattening and a small island of inferior central flattening
Keratoconus
- Munson's sign (lower lid bulge on downgaze)
- Rizzuti's sign (loss of normal corneal reflectance in the slit lamp)
- retinoscopy scissors reflex
- Charleaux oil droplet sign (retroillumination)
- Vogt's striae (folds in Descemet's membrane)
- Fleischer's ring (iron in corneal epithelium)
- stromal thinning
- stromal scarring
- prominent corneal nerves
- swirl SPK staining
- pseudo-reduced IOP
- loss of BCVA
- asymmetric (>1D) astigmatism
- elevated total higher-order aberrations
- elevated vertical coma (> 0.53 um)
- elevated topography I/S values (>1.4)
- apical elevation over best fit sphere on anterior and posterior elevation maps
- corneal thinning
- corneal irregularity
Cornea ectasia
- certain patietns have a genetically different type of collage composition of their cornea that predisposes them to ectasia (external factors such as eye rubbing, RGP wear and refractive surgery may trigger the process of thinning)
- insult to collagen corneal fibrils via surgery, trauma, RGP wear or eye rubbing causes the corneal matrix to lose structural integrity
Rosacea treatment
Oracea (30mg immediate release, 10mg of slow release doxycycline) -- QAM on empty stomach or at least 1 hour prior or 2 hours after meals
MetroCream 0.75%
-use sunscreen to prevent sunburns
-can cause GI distress
Monday, February 11, 2008
AzaSite "pink eye" drop
recommended dosage: BID x 2 days, QD x 5 days (total of 9 drops vs. 21 other brands)
demonstrated prolonged high levels in ocular tissue
good for bleph/bacterial conjunctivitis/dry eye patients (exerts anti-inflammatory activity along with antibacterial activity)
Acetaminophen dosages
>2 mo. (5kg): 80mg per dose
>4 mo. (6.5 kg): 100mg per dose
>6mo. (8kg): 120mg per dose
>12mo. (10kg): 160 mg per dose
>2 years (13kg): 200mg per dose
>3 years (15kg): 240mg per dose
>5 years (19kg): 280mg per dose
well-hydrated child: 15 mg/kg q4-6hrs
dehydration risk: 10 mg/kg q4-6hrs
maximum: 90 mg/kg/day (up to 4 grams daily)
Thursday, February 7, 2008
Pyogenic granuloma
- benign vascular lesion of the skin and mucosa
- appear as a fleshy red mass with relatively rapid growth
- Histology: mixed acute and chronic inflammatory cells, with capillary proliferation in a lobular pattern (capillary hemangioma)
- occurs most often in children and pregnant women and may occur close to the site of a minor injury
- causes: usually associated with some inflammatory process such as a chalazion, severe blepharitis and meibomianitis, as a foreign body reaction or trauma such as surgery (pterygium excision, chalazia incision and drainage, placement of orbital implants, nasolacrimal duct probing with silicone tube placement, insertion of silicone punctal plugs, blepharoplasty, and eye muscle surgery).
- in most cases, these lesions will resolve with topical steroid administration x2-3 weeks
- surgical excision may be required for those lesions that fail to resolve after topical treatment
- in rare cases malignant neoplasms such as Kaposi’s sarcoma may mimic pyogenic granuloma
- recurrence following excision is extremely rare
CRAO
Symptoms:
- abrubt, painless vision loss (pain = OIS)
- amaurosis fugax precedes visual loss in 10% of patients
- men:woman = 2:1; mean age = 60; bilateral involvement = 1-2%
Findings:
- VA 20/800 to LP (NLP = ophthalmic artery obstruction or temporal arteritis)
- +APD
- anterior segment normal (except if OIS, can have NVI)
- ischemic whitening of the retina
- cherry red spot at macula
- ONH pallor with splinter retinal hemorrhages
- 20-25% demonstrate visible emboli
Differential diagnoses:
- mild, nonischemic CRVO
- neuroretinitis
- hypertensive retinoathy
Sequelae:
- after 4-6 weeks, retinal whitening dissipates, leaving optic nerve pallor
- arterial collaterals
- absent foveal reflex
- RPE hyperplasia from stress to the RPE
- NVI/NVG = 18% (make referal for panretinal laser photocoagulation)
- after >100 minutes, complete irreversible loss
Causes:
- Blood conditions: coagulopathies or poor blood flow, antiphospholipid antibody syndrome, protein S deficiency, protein C deficiency, antithrombin III deficiency
- Systemic disease: 60% of patients have HTN, 25% have DM, 50% no cause identified
- Heart disease: 30% have carotid artery disease; Refer patients (especially those <50> 50 y/o
- Optic neuritis
- Local trauma producing damage to the optic nerve
- Radiation exposure
- Behcet disease
- Migraine
- Syphilis
- Optic disc drusen
- Prepapillary arterial loops
Management:
- 350mg ASA, agressive digital ocular massage, topical beta blocker, oral Diamox 2 x 250mg (attempt to lower IOP to decrease resistance to nerve and retinal blood flow), breath into brown paper bag (stimulate rtinal arterials)
- Labs:
- CBC w/ differential and platelets
- blood pressure
- fasting BS
- lipid panel
- cholesterol
- ESR (if yes, requires high-dose corticosteroid treatment)
- CRP
- HLA-B27
- FTA-Abs
- HIV
- electrocardiogram with 2-D echo
- transesophageal electrocardiogram
- carotid doppler
- MRI
Tuesday, February 5, 2008
msd Mini-Scleral Design (from Blanchard CL company)
- designed to vault the cornea and fit on the sclera/conjunctiva, reducing the net-vault of the contact lens over the cornea
- reduction in the chance of irritation and better centering
- keratoconus fits that dont center or dislodge with eye mvmt
- irregular cornea fits
- GP-intollerant patients (chronic awareness)
- sagital depth of the CL
- trial fit progressively deeper vaults until corneal clearance achieved
- compression ring on conjunctiva after full day wear is ok
- if mid-peripheral or limpal touch exists, increase the mid-peripheral zone of the lens to move the surface of the lens off the cornea
- if mid-peripheral space b/w lens and cornea is too great (causing an air bubble), which may cause epithelial desiccation, decreasing the mid-peripheral zone will minimize these issues
- small air bubbles in periphery that move during lens wear don't interfere with vision or cause epithelial surface drying
Tears Again Hydrate
- for dry eye, blepharitis, MGD
- Rx only
- omega-3 fatty acid, flaxseed oil, evening primrose oil, omega-6, bilberry extract
- anti-inflammatory properties
- 4 soft gels daily, directly or during meals/snacks
- avoid taking at the same time with other medications or supplements, or if pregnant/nursing
- possible side effects: intestinal blockage, thyroid problems, may reduce blood vessel platelet aggregation (if you're taking ASA or blood thinners have your clotting time checked, may lower the seizure threshold in patients taking seizure meds
Saturday, February 2, 2008
Visual Fields - documenting progression
- change in the total deviation values over time may be due to factors other than glaucoma such as advancing cataract or decreased pupillary size.
- by using the pattern deviation values, the GPA software specifically targets the localized change associated with glaucoma
- If there were a diffuse component to the glaucomatous change, it would not be reflected in the GPA result, but the more likely localized component due to the formation of new glaucomatous defects or the expansion and deepening of existing defects would be characterized
- change needs to be present in 3 consecutive visual fields before progression can be confirmed
- if progression has occurred and there is a resultant change in therapy, the clinician should
establish a new baseline so that any additional progression can be found - if the patient undergoes ocular surgery or develops another ocular condition, new baseline
tests after he stabilizes should be selected for use in evaluating subsequent examinations
- gives the slope associated with change in the mean deviation
- this change will include anything that affects the subject’s visual sensitivity, including advancing cataract, and that it may not reflect change due to glaucoma.
- The GPA software will automatically assess the next visual field (and the next) to determine if that change is repeatable.
- If it is present on two consecutive tests, a half-filled triangle will appear at the location
- For repeatable change on three consecutive tests, a closed triangle will appear.
- The GPA software then assesses the repeatability of three or more points and gives a plain-language report of “possible progression” if two consecutive fields show that
- the same three or more points changed from baseline or “likely progression” if three consecutive fields show change at the same three or more points.
Thursday, January 31, 2008
Retinal hemorrhages
- located on retinal surface
- subhyaloid hemorrhage is located b/w the posterior vitreous base and the internal limiting membrane (ILM)
- preretinal hemorrhage is located posterior to the ILM and anterior to the NFL
- "boat-shaped" with sharp demarcation line
- obscure retinal features
- tend to clear quickly without any sequelae
- associated with pathology affecting the major retinal vessels or superficial beds
- most common etiology: retinal neovascularization
- other etiologies: PVD, retinal breaks, associated with the tearing of a mjor retinal vessel
- less common etiologies: Terson's syndrome, retinal trauma, valsava retinopathy
Flame-shaped hemorrhages (NFL hemorrhages)
- located within the NFL
- flame shape is the result of the structure of the NFL
- typically located in the posterior pole
- tend to resolve within a 6 weeks
- associated with retinal vasculature pathology affecting the superficial and peripapillary capillary beds
- etiology: hypertensive retinopathy (AV nicking present), retinal vein occlusions, optic neuropathy (papilledema, NTG, anterior ischemic optic neuropathy)
- Roth spot = flame-shaped hemorrhage that has a white or pale center; represent non-specific signs of blood dyscrasias (anemia/thrombocytopenia, anoxia, AV malformation, bacterial endocarditis, collagen vascular disease, diabetic retinopathy, HIV, HTN retinopathy, leukemia, multiple myeloma, trauma)
Dot-and-blot hemorrhages
- located in the retina's inner nuclear and outer plexiform layers
- configuration is due to intraretinal compression
- take longer to resolve because they're deeper than flame-shaped hemorrhages
- commonly associated with microvascular signs of edema
- etiology: pathology affecting the prevenular capillaries -- diabetic retinopathy, idiopathic juxtafoveal retinal telangiectassis, vein occlusion and OIS
- OIS: vascular insufficiency associated with carotid artery disease leads to ocular hypoperfusion --> not enough pressure to push blood from retinal arterioles to the venules --> increased capillary congestion results in a breakdown of the capilary walls with subsquent hemorrhage and edema --> venules attempt to compensate for the decreased blood flow by distending, giving them a dilated, but non-tortuous appearance
Subretina and subretinal pigment epithelium (RPE) hemorrhages:
- located beneath the neurosensory retina and the RPE
- sub-RPE hemorrhages are located b/w the RPE and Bruch's
- exhibit a dark coloration with the retinal vessels clearly visible above
- tend to have an amorphous shape, due to the absence of firm attachments b/w the neursensory retina and RPE, allowing the blood to spread
- sub-RPE hemorrhages have well-defined borders attributed to the tight cell junctions among RPE
- may be associated with neurosensory or RPE detachments in the posterior pole
- tend to resolve slowly
- may be associated with the functional and/or structural changes at the level of the photoreceptors (therefore, unfavorable prognosis)
- most common etiology: CNV
- other etiologies: choroidal tumors, trauma, retinal angiomatous proliferation
- referal to a retinologist
Management
- referral if needed
- patients without systemic history need medical work-up (most common etiologies: HTN, DM; other: clotting disorders such as hemophilia or patients on warfarin)
- fasting plasma glucose test (<100> 126 is indicative for diabetes)
- HbA1c (normal <5%)
- CBC with white cell differential (test for anemias, polycythemias, bleeding disorders, leukemias, infections)
- prothrombin time (PT) and international normalized ratio (INR) -- evaluates clotting factors
- OIS: work-up of above plus heart echo, carotid USG and/or Doppler color imaging to rule-out carotid or heart disease
- in older patients (>60) -- ESR & C-reactive protein & temporal artery biopsy to confirm
- in younger patients (18-40) -- at risk for blood dyscrasias, diabetes, HTN, hyperlipidemia -- obtain a serum lipid profile, consider antiphospholipid and anticardiolipin enzymes to determine whether they have antiphospholipid syndrome; ANA or double-stranded DNA testing to r/o Lupus; ANA & ESR screening test for autoimmune diseases and inflammatory conditions
- other tests: HLA-B51, HLA-B27, HLA-B5, ELISA, Western-blot specific testing for HIV, Lyme disease, toxoplasmosis, tuberculosis
- other tests: FTA-Abs and RpR to r/o syphilis
- other tests: blood cultures to identify widespread infection (speticemia)
Retinal vasculature anatomy
- Carotid artery --> ophthalmic artery branch --> branches into the CRA (blood supply of the inner retina) --> branches in NFL to all quadrants except the foveal avascular zone
- choroidal vasculature supplies nutrients and oxygen to the macula
Punctal plugs codes
from: http://www.ocusoft.com/OcclusionTherapyRateCharts/CaiforniaRestofState.pdf
Diagnostic Codes used to characterize Lacrimal System Dysfunction:
- Tear Film Insufficiency 375.15
- Keratoconjuctivitis Sicca 370.33
Redness or Discharge 379.93 - Pain in or around eye 379.91
1st VISIT (LO1) - Lacrimal EfficiencyTesttm with dissolvable Collagen / CollaSyn™ test plugs in upper and lower puncta
- Occlude left upper punctum with test plug 68761-E1
- Occlude left lower punctum with test plug 68761-E2
- Occlude right upper punctum with test plug 68761-E3
- Occlude right lower punctum with test plug 68761-E4
- 10 Day Post-Operative Period
2nd VISIT (LO2) - Non-Dissolvable or 6 Month Dissolvable VisiPlug™ Lacrimal Plugs in upper puncta, re-test lower puncta
- Occlude left upper punctum 68761-E1
- Occlude right upper punctum 68761-E3
- Occlude left lower punctum with test plug 68761-E2
- Occlude right lower punctum with test plug 68761-E4
- 10 Day Post-Operative Period
3rd VISIT (LO3) - 6 Month Dissolvable VisiPlug™ Lacrimal Plugs® in lower puncta
- Occlude left lower punctum 68761-E2 3
- Occlude right lower punctum 68761-E4 3
RELATED CPT CODES
- Probing of canaliculi, with / without irrigation,Plug Repositioning or Removal (L04, L05) 68840
- Dilation of punctum, with / without irrigation, Plug Removal (LO5) 68801
- Probing of nasolacrimal duct, with / without irrigation, Plug Removal (LO5) 68810
Tuesday, January 29, 2008
Combigan
- dual mechanism of action to lower IOP by reducing aqueous-humor production and enhancing aqueous-humor drainage/outflow
- BID dosing
- mean decrease from baseline IOP 4.4-7.6mm HG with Combigan (vs. 2.7-5.5 with brimonidine tartrate, vs. 3.9-6.3 with timolol)
- maintained mean IOP throughout day better than individual gtts
- mean daytime IOP was consistently <18>
- systemic absorption helps to control for crossover effects of the drugs and controls for asymmetric fluctuations of IOP b/w right and left eyes
- mean daytime decrease from baseline IOP was >20% in 42% of Combigan patients, 13% brimonidine, 27% timolol
- lower incidence of conjunctival follicles compared to brimonidine (but higher than timolol group)
- rate of discontinuation for adverse effects was 14% with Combigan (vs. 30.6 with brimonidine vs. 5.1% with timolol)
- rate of allergic conjunctivitis was 5.2% with Combigan (vs. 9.4% brimonidine vs. 0.3% timolol)
- contraindications: patients with bronchial asthma, sinus bradycardia, severe COPD, overt cardiac failure, cardiogenic shock, atrioventricular block
Monday, January 28, 2008
DLK after LASIK
- inflammatory cells (eosinophils, neutrophils, lymphocytes) that migrated underneath the LASIK flap
- leads to collagenolytic activity that weakens the corneal structure and leads to stromal melting and ectasia
- 0.2%-5.3% incidence
- occurs in both mechanical microkeratome and IntraLase procedures
- usually due to bacterial endotoxins released from sterilizer reservoirs
- can occur as soon as 24 hours after surgery or as a late-onset problem, occuring many months after surgery
- increased risk: epithelial defects after surgery or patients who have atopic disease
Signs/symptoms:
- symptoms may mimic dry eye
- grainy appearance b/w the flap and underlying stromal bed
- only mildly hyperemic conjunctiva
- no ciliary flush like infectious keratitis
- as severity increases, may cause decrease in VA, irregular astigmatism, ectasia, hyperopia
Treatment:
- Pred Forte q1-2hour, follow-up every day until improves
- topical fluoroquinolone tid prophylaxis if needed
- cyclopentolate for pain
- severe cases need referral back to surgeon to lift flap and irrigate the area with sterile balanced salt solution to remove inflammatory cells
- severe cases oral prednisolone 40-80mg per day for at least one week
Corneal transplant examinations
- redness
- irritation,
- light sensitivity
- FBS
- blurred vision
- general inflammatory response (vascular dilation and transudation)
- cellular infiltration -- sub-epithelial infiltrates ~0.5 mm scattered throughout the donor tissue only (respond to topical steroids)
- tissue edema
- stromal rejection -- neovascularization and stromal infiltrates
- endothelial rejection -- KPs scattered across the endothelium or in a linear form advancing in from the peripheral cornea; causes edema of stroma and epithelium
GP fittings
- intermediate (8.6-9.2) --> Flat K
- large (9.3-10.2) --> 0.50 flatter than flat K
- small (8.0-8.5) --> 0.50 steeper than flat K
Adjust for corneal toricity:
- steepen slightly if toricity is between 1.25D and 2.ooD
- consider toric design if >2.00 corneal toricity
Misc
- steepen the GP if the lens rides nasally or temporally
- flatten the GP if it rides inferiorly
- increase the optical zone and overall diameter if the GP rides superiorly
Piggyback fittings:
- observe for excessive apical bearing or superior alignment with seal off of a GP (results in a "swirl staining")
- select high-DK silicone hydrogels
Sunday, January 27, 2008
OHTS findings
- At 5 years: observation group = 9.5%, treatment group = 4.4% developed glaucoma
- At 7 years, observation group = 13%, treatment group = 4.4% developed glaucoma
Risk factors for developing POAG identified:
- advanced age
- race (the prevalence of glaucoma is higher in blacks than in whites)
- sex (male)
- larger vertical cup-to-disc ratios
- greater pattern standard deviation on Humphrey visual fields
- thinner central cornea measurements.
- IOP fluctuation and Diurnal curves -- peak IOP at night
- systemic disease
- optic nerve hemorrhages
- PPA
- zone alpha -- further from the disc; chorioretinal/pigment crescent
- zone beta -- adjacent to disc; scleral crescent (more associated with glaucoma)
- sleep apnea
- high myopia (structural changes make it hard to evaluate nerve shape)
Glaucoma risk calculators
http://www.discoveriesinsight.org/grc_web/grc.cfm
WashU:
http://ohts.wustl.edu/risk/calculator.html
American Academy of Ophthalmology definition of glaucoma:
"A multi-factorial optic neuropathy in which there is characteristic acquired loss of retinal ganglion cells and atrophy of the optic nerve." (This definition allows for the presence of glaucoma in the absence of visual field loss, and does not even address IOP. )
NTG = 1 out of 6 POAG patients